Our thoughts and fears, movements and sensations all arise from the electrical blips of billions of neurons in our brain. Streams of electricity flow through neural circuits to govern these actions of the brain and body, and some scientists think that many neurological and psychiatric disorders may result from dysfunctional circuits.
As this understanding has grown, some scientists have asked whether we could locate these faulty circuits, reach deep into the brain and nudge the flow to a more functional state, treating the underlying neurobiological cause of ailments like tremors or depression.
The idea of changing the brain for the better with electricity is not new, but deep brain stimulation takes a more targeted approach than the electroconvulsive therapy introduced in the 1930s. DBS seeks to correct a specific dysfunction in the brain by introducing precisely timed electric pulses to specific regions. It works by the action of a very precise electrode that is surgically inserted deep in the brain and typically controlled by a device implanted under the collarbone. Once in place, doctors can externally tailor the pulses to a frequency that they hope will fix the faulty circuit.
The FDA has only approved deep brain stimulation for a handful of conditions, including movement disorders — dystonia, essential tremor and symptoms of Parkinson's disease — and a type of treatment-resistant epilepsy. Now, many scientists in the U.S. and around the globe are experimenting with the technology for psychiatric conditions like depression or obsessive-compulsive disorder.
The results of clinical studies so far are very mixed: Some patients say they have been totally transformed while others feel no effect at all, or they get worse.
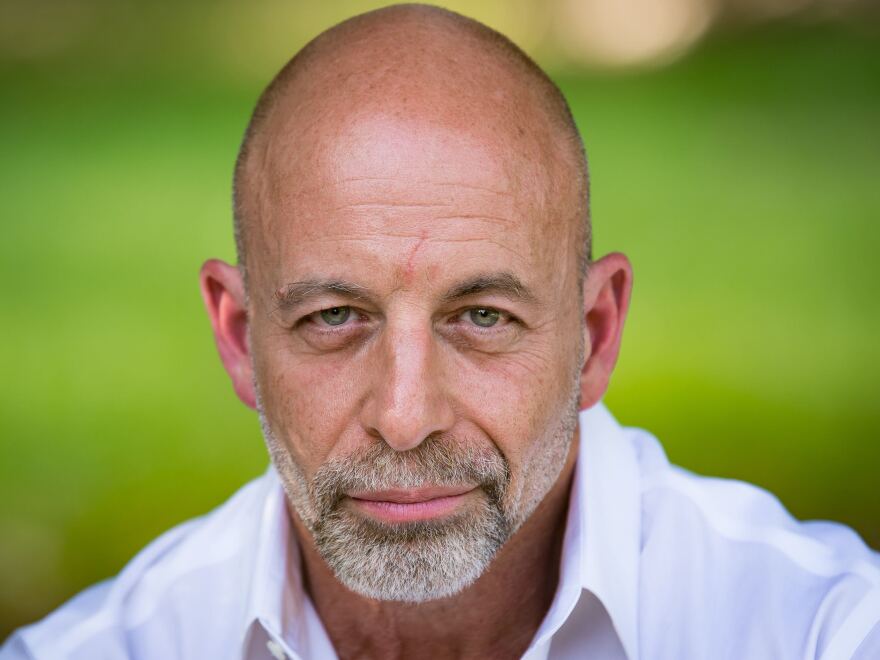
Yet research continues and the technology's potential to instantly and powerfully change mood raises ethical, social and cultural questions. NPR spoke to neuroethicist, James Giordano, chief of the Neuroethics Studies Program at Georgetown University Medical Center, about this new technology and its potential benefits and harms when used for psychiatric treatment. In addition to his work at Georgetown, Giordano has consulted with the U.S. military about these technologies and their possible use.
This interview includes answers from two separate conversations with Giordano, one conducted by Alix Spiegel and one by Jonathan Lambert. It has been edited for clarity and length.
What is deep brain stimulation and how does it work?
Scientists have been stimulating brains for a while now, but it has historically been quite crude. A neurosurgeon [would] touch a brain area with an electrode, and see what happened, what types of functions were affected. But we didn't have a detailed picture of what we wanted to target in the brain, and the electrodes themselves were not very precise.
Now we have a much more detailed map of the networks and nodes of neurons involved in different pathologies [like Parkinson's, obsessive-compulsive disorder, etc.] or different thought patterns or emotions. Deep brain stimulation provides a fairly specific and very precise way to utilize electrodes to deliver electrical current in and around a small set of brain cells to turn them on or modulate their activity.
Modify the circuit, and you can modify the behavior. The goal is to use DBS to modify the circuits in such a way as to improve symptoms in a very specific and precise way.
How do you know what kinds of specific inputs you want the electrode to a deliver, and where in the brain to deliver them?
There's an old adage in brain science: "When you've seen one brain, you've seen one brain." This is certainly true, but all brains have a lot of similarity on which individual variation is built because brain structures are changed and developed as a consequence of experience.
So when implanting a device, we know generally where we're going, but because the patient is awake while we're implanting the device, we can further tailor it to know where precisely to put it for the desired effect. More fine-tuning, in terms of the kind of stimulation to provide, can be done after surgery, because the device can be tuned externally.
Though it's not yet FDA approved for them, there is ongoing research on treating psychiatric disorders with DBS? What is the research finding so far?
Many studies are certainly finding evidence that DBS can be effective for treating disorders like Tourette's syndrome, obsessive-compulsive disorder, and even depression. Patients are reporting a reduction in the symptoms, but we certainly still have many questions that need answering. For example, when do we treat with DBS? Early in the development of a disorder? Later, after other options have been exhausted? These are questions that still need answering.
How would you explain the difference between how an antidepressants affects the brain and how deep brain stimulation works?
A drug like Prozac or antidepressant drugs is basically like throwing water on your face to get a drink of water. Using something like deep brain stimulation is like putting a drop of water on your tongue. We can increase the specificity and precision ... and, in many ways, the precision and specificity of deep brain stimulation makes it a more effective tool. It can be turned on and turned off. It can be adjusted in the very short term so it can be a more flexible tool that allows a much more precise control of mood.
And compared with antidepressants, are there differences in moral or ethical implications in the use of a treatment that allows us to act so specifically on mood?
Specificity is power. And the moral obligation that comes with great power is overwhelming. The responsibility to understand as best as conceivably possible what you're doing not only on a neurobiological level, but also on an existential and even social level. What are you doing? Are you creating new normal [in terms of mood]? And if you're creating new normal, do we have what I'll call "the ethical equipment" on board to be able to address this? In some cases I think the answer is yes, but I think in other cases what you're going to begin to see is that new ethical principles may need to be developed because of the potential and reality of the way these things are being used.
For example, expressive creativity. Is there an ethical principle of self-creativity ... that I can define myself and say I want to create myself in these ways?
Do you mean, theoretically, in the future, you could go to a doctor and say I want to be a great artist?
Now we're not quite to that point, but I could certainly go to a physician and say I want to be more outgoing, I want to be less inhibited. I'd like to be happier on a daily basis. I'd like to feel more enlightened in my daily experiences ... In an open society, are we saying that one should be able to define 'I want to be this' and this is a tool to get there? Perhaps, but then we also have to balance that. What about others? ... This gets back to a question of fairness. Can everybody get this? Who's going to get this?
What can go wrong with this technology? What should we be worried about?
Well, it is neurosurgery, and there are certainly risks that go along with that, infection, problems with the procedure. Targets could be missed or misidentified. Those are risks that come with the territory.
But there are some more cases more specific to DBS. What if you get effects that you didn't anticipate? By stimulating Area X, it's possible that we could get a spillover effect that modulates other things ancillary to that, like personality, temperament, character, personal preferences. There have been case reports and anecdotal reports of things like that happening, but they're rare.
So could implanting a DBS device have some unanticipated consequences for our tastes or personal characteristics like introversion and extroversion?
One of the better-known cases, for example, was a person whose musical taste had nothing to do with country music. And after a deep brain implant for a movement disorder, [the person] developed a real pathos for Johnny Cash music and was just totally into the aesthetic of Johnny Cash. Is it possible for these things to occur? Of course, it is. The brain works as a coordinated set of nodes and networks that are intercommunicative and reciprocal. So changing the local field electrical activity in one area isn't necessarily going to be completely discrete from the wiring, if you will, of the kind of activities and the functions of other brain areas. These things occurring up- and down-stream represent real effects.
Can treatment with a DBS device change more than just our mood, but also our personality?
Yes, although we have to ask ourselves whether those changes are due to the positive consequences of DBS. If someone with Tourette's was an introvert, and then they get a DBS implant and become more of an extrovert and more socially engaged, is this a side effect of the DBS? Or because they're no longer bearing the burden of being someone with a constant verbal tic?
DBS also raises questions of personal autonomy. Are we going to get cases of people saying "my deep brain stimulator made me do it"? Perhaps. But very often patients report that the condition they had which DBS is treating impaired their autonomy more than they feel the deep brain stimulation is.
What guidance would you give doctors working with DBS in a patient? Because they can affect the state of someone's mood by the levels of the electrical current in the device, how do they know what level to set?
To the point of clinically relevant therapeutic improvement. Just as one would set for example the levels that one could use through any other therapy, [like] cognitive behavioral therapy. Is the person functional? Are they saying, "yes I feel better, my mood is better." The same would be true of a drug, however this is more powerful because you're directly affecting those nodes and networks that appear to be some substrate of the thing that causes this person's mood. So you want to be cautious. The general tenor in the field is start low and go slow.
Beyond DBS, where this might this technology ultimately go?
There is a do-it-yourself market if you will, for not deep brain stimulation but transcranial electrical stimulation. What that's showing is that there is an increased interest in neurotechnologies that are not just oriented toward alleviating a medical condition but that change key aspects of cognition, emotions and behavior. This is sometimes referred to as the cosmetic use or designer use of neurotechnology. [If] I don't like key aspects of personality, [such as being shy], could I modify that for example through the use of these neuro technologies? Those things are coming and it's not in the near future — there's interest now.
What pitfalls do we face if this technology becomes more widely used?
Mistakes will get made. Hopefully, we'll be bright enough to correct them and recognize them when they occur not only in terms of the technological and scientific mistakes but ethical, moral, legal mistakes. In many ways, this represents something of a brave new world of capability. And I think that we have to be very, very sentinel to what the potential of this could yield. Yeah this could yield some really wonderful things but also, along with that, if it's used for cosmetic purposes like self-enhancement, could this lead to potentially violent outcomes? I can guarantee you that things that are at very, very problematic and, in some cases, devastating will occur. Do I believe that the net effect will be beneficial because we will respond appropriately to those mistakes that we make? Yeah that's my hope. Do I know that we will? I don't know.
Copyright 2021 NPR. To see more, visit https://www.npr.org. 9(MDA1MTkyNjA1MDEyNzM1MTQ0ODk3NTA1NA004))




